Medically reviewed by Dr. Kerac Falk, MD, FACOG.
Navigating the world of healthcare coverage can seem daunting and complex, often leaving us with more questions than answers. But for those dealing with or caring for someone with incontinence, finding reliable and affordable solutions is paramount.
Absorbent incontinence supplies and hygiene items can improve the quality of life for seniors with incontinence. However, seniors on fixed incomes may be understandably concerned about the ongoing expense of purchasing adult diapers, absorbent pads, and other incontinence supplies.
This concern naturally leads to the question, “Are incontinence supplies covered by Medicare?” Let’s take an in-depth look at Medicare coverage for incontinence supplies, other potential options that may be available, and how to access the resources you need.

Does Medicare Cover Incontinence Supplies?
Unfortunately, Medicare does not currently offer coverage for any absorbent incontinence supplies or hygiene items. This includes things like incontinence underwear, pads and guards, as well as wipes and other incontinence skincare.
Original Medicare is a national program, so this rule remains consistent from state to state. With as many as 13 million people in the US experiencing urinary incontinence, many older adults must pay out of pocket for the supplies they need. But don’t lose hope! There are some other options to consider.
Understanding Medicare Coverage for Incontinence Supplies
Medicare Parts A, B, and D do not cover any incontinence supplies. However, there are some Medicare Part C, also called Medicare Advantage, plans available in various parts of the country that offer OTC benefits, which may extend to incontinence supplies, including bladder protection items and hygiene products.
Medicare Part C plans are offered by private insurance companies with Medicare approval, and they are only available in specific areas. If there are Medicare Part C plans available in your area, a careful review of the summary of benefits will help you determine if the coverage extends to incontinence care.
It’s also important to know that Medicare Supplement, or Medigap, plans do not provide any coverage for incontinence supplies. These supplement plans are secondary to Original Medicare and don’t provide additional benefits beyond what’s covered in the original plan.
On the other hand, if you have both Medicare and Medicaid, Medicaid may cover certain incontinence supplies. However, Medicaid is a state-run program, and coverage will vary from state to state.
Does Medicare Cover Adult Diapers for the Elderly?
Medicare does not pay for adult diapers or any other form of OTC disposable supplies needed for elderly care, including things like bandages and gauze. Individuals who require these types of common medical supplies will be responsible for purchasing their supplies out of pocket or turning to other resources for assistance.

Does Medicare Advantage Pay for Adult Diapers for Seniors?
Medicare Advantage plans, offered by private insurance companies approved by Medicare, may offer coverage for adult diapers and other incontinence supplies for seniors. These plans can vary in coverage, so it’s advisable to review your documentation or contact the plan administrator to understand the extent of coverage your specific plan provides.
If your Medicare Advantage plan does cover adult diapers, be sure to read the summary of benefits closely to determine any cost or quantity limitations. In many cases, only a portion of your incontinence supplies for a given year will be covered.
To obtain coverage for incontinence supplies through Medicare Advantage, your doctor will need to write a medical justification statement that explains why the supplies are necessary. Your healthcare provider and supplier can walk you through this process.
Does Medicare Cover Incontinence Treatment?
Yes, Medicare does typically cover medical treatments for conditions that cause or contribute to incontinence. This could include equipment, medications, procedures, or therapies aimed at addressing underlying causes of overactive bladder, chronic urinary tract infections, and other related issues.
Some examples include:
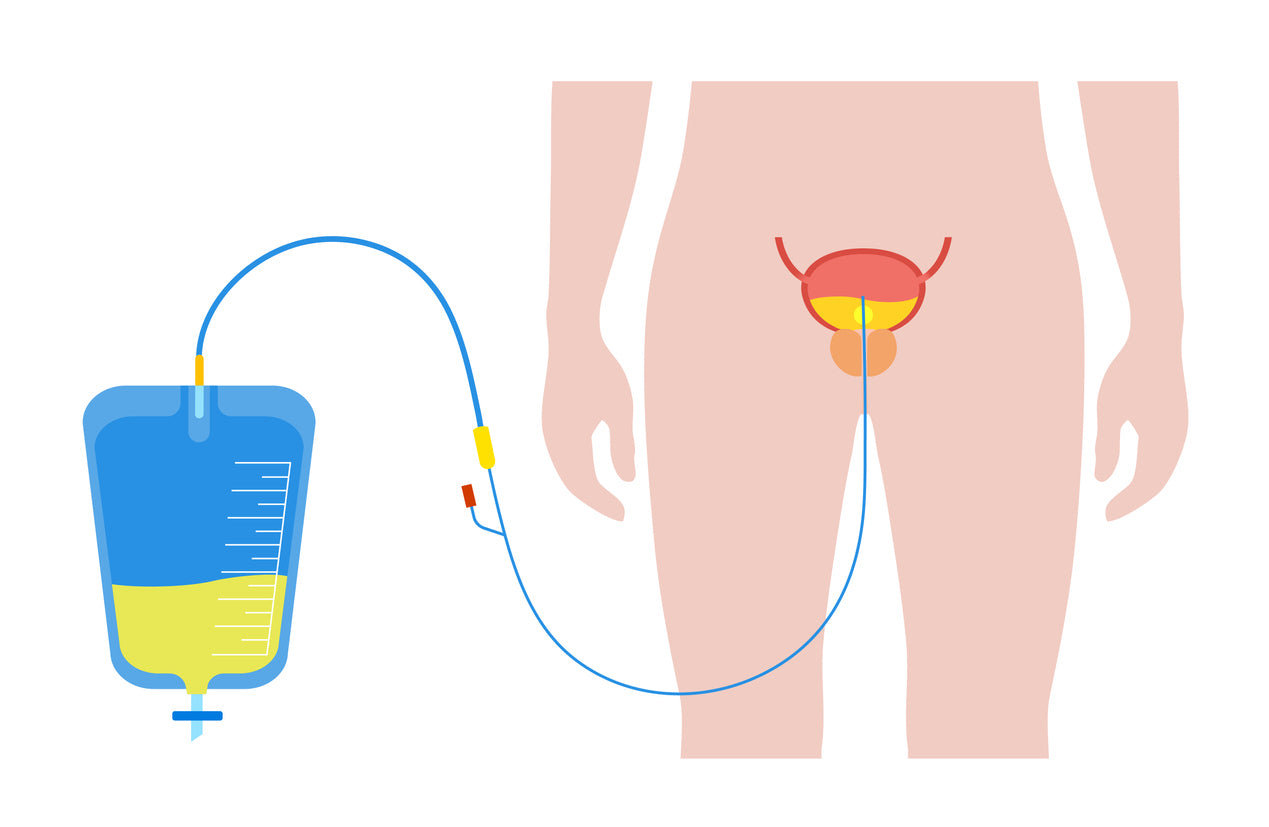
- Durable Medical Equipment: If your healthcare provider has prescribed catheters for permanent urinary incontinence or urinary retention, Medicare may reimburse you for up to 200 catheters each month. Coverage may also be available for things like commode chairs and mobility devices if they are considered medically necessary and fall under the category of Durable Medical Equipment (DME).
- Pelvic Devices: Certain pelvic devices designed to reduce the symptoms of incontinence may be covered by Medicare, but only if they’re prescribed by your doctor.
- Incontinence Control Devices: Medicare may cover incontinence control devices, such as collagen implants or sacral nerve stimulation devices, which can improve bowel and bladder control.
- Biofeedback Therapy: Biofeedback-assisted pelvic muscle training may be covered by Medicare. This therapy is used to improve awareness in the pelvic floor muscles to reduce the symptoms of incontinence.
- Surgical Procedures: If your doctor recommends surgery to treat incontinence, such as bladder sling surgery, it may be covered by Medicare.
- Incontinence Medications: Your doctor may prescribe medications to help with incontinence-related conditions and symptoms. Your Medicare Part D drug plan may help to cover some of the costs of these medications, but you will be responsible for any deductible, coinsurance, or copayment required out of pocket.
Coverage specifics can vary, so it’s important to consult with your healthcare provider and plan administrator for precise information.
What Will Medicare Not Pay For?
Medicare does not cover any supplies that are not considered medically necessary, such as items for comfort or convenience. Additionally, disposable items and items used primarily for hygiene, such as wipes or cleansers, are not covered.
Why Doesn’t Medicare Cover Incontinence Supplies?
Medicare only covers items that are considered medically necessary. Adult diapers, pads, briefs, and other absorbent incontinence supplies do not fall into this category. However, they will typically cover medically necessary treatments and procedures related to the diagnosis and care of incontinence-related conditions.

How To Get Free Diapers for the Elderly?
Nonprofit organizations, local community programs, and state assistance programs may offer support for elderly individuals in need of free incontinence supplies. Reaching out to local organizations through Area Agencies on Aging, which is dedicated to helping older adults remain in their homes, can guide you toward available assistance.
Diaper banks may also provide free incontinence supplies to seniors who need assistance. Because Market partners with the National Diaper Bank Network, which includes diaper Bank programs in every state.

Ways to Save Money On Incontinence Supplies
For those seeking assistance beyond Medicare coverage and local organizations, there are several ways to save money on incontinence supplies.
Shopping online, signing up for a recurring subscription, and buying in bulk can help you save money on incontinence supplies. Plus, your items will be delivered right to your door, saving you time and money for gas or public transportation.
Additionally, some discount prescription drug cards may cover certain incontinence supplies.
Wrapping Up
Although Medicare does not cover incontinence supplies, there are other resources available for seniors who need assistance. Most importantly, seniors with incontinence should not try to change their bladder protection products less frequently in an effort to save money. This practice could cause skin and hygiene issues, which may lead to additional healthcare expenses.
Are you struggling with incontinence? Take our bladder protection quiz to figure out what product might work best for you and get a sample pack to try!
Take the Quiz
About the Expert:
Dr. Falk is a fellowship-trained urogynecology subspecialist, double board-certified in both Obstetrics and Gynecology, as well as Female Pelvic Medicine and Reconstructive Surgery. He has expertise in the treatment of female pelvic floor disorders, which encompass many common but infrequently-discussed conditions which significantly impact women’s quality of life. These include complex disorders such as urinary and bowel incontinence, pelvic organ prolapse, childbirth injury, genital fistulas, recurrent urinary tract infection, and bladder pain.
Sources:
Medicare.gov. (n.d.). Incontinence supplies & adult diapers. Retrieved from https://www.medicare.gov/coverage/incontinence-supplies-adult-diapers
Illinois Department of Public Health. (n.d.). Incontinence. Retrieved from http://www.idph.state.il.us/about/womenshealth/factsheets/inc.htm#:~:text=Who%20is%20affected%20by%20incontinence,most%20common%20among%20the%20elderly.
































