Stroke survivors often face a range of challenges during their recovery journey, and one significant aspect is managing incontinence issues. One study found that more than 80% of stroke survivors reported one or more abnormal urinary symptoms at 3 or 12 months post stroke. Another study found fecal incontinence to be prevalent in 30% of survivors 7 to 10 days post stroke, 11% at 3 and 1 year, and 15% at 3 years. However these challenges can be made easier through practical strategies, medical insights, and supportive resources designed to help individuals and their caregivers navigate the complexities of stroke-related incontinence.
Can a Stroke Cause Incontinence?
Yes, a stroke can cause incontinence. When a stroke occurs, it can disrupt the brain's control over various bodily functions, including those related to bladder and bowel movements. The extent and type of incontinence depend on the location and severity of the stroke. Commonly, strokes may affect the nerves and muscles responsible for maintaining urinary and fecal continence, leading to difficulties in controlling bowel and bladder function. Seeking prompt medical attention and rehabilitation can play a crucial role in managing and improving incontinence issues associated with stroke.
Understanding Stroke Incontinence
Stroke incontinence can take many forms and is not always limited to the bladder. It is crucial to recognize that not every stroke survivor experiences incontinence, and its occurrence does not automatically attribute causation to the stroke itself. This section delves into the diverse types of incontinence commonly linked with strokes, the intricate relationship between stroke and bladder as well as bowel functions, and the prevalent signs and symptoms that warrant attention in understanding and addressing post-stroke incontinence.
Types of Incontinence Associated with Stroke
Several types of incontinence are commonly associated with stroke, reflecting the diverse ways in which stroke-related neurological changes can impact bladder and bowel control. One prevalent type is urge incontinence, characterized by a sudden and intense need to urinate or defecate, often leading to involuntary leakage. Stress incontinence is another common form, wherein pressure on the bladder or bowel during activities like coughing or lifting triggers leakage. Overflow incontinence may occur when the bladder does not empty completely, resulting in dribbling or constant leakage. Additionally, individuals may experience functional incontinence due to physical or cognitive impairments hindering their ability to reach the restroom in time.
Nocturia or nocturnal enuresis can also occur either on their own or as a result of another form of incontinence. For example, if you suffer from urge incontinence, you may also struggle with nocturia if it occurs throughout the night.
Reflex incontinence is when a person experiences a sudden loss of urine without warning. Ordinarily, the bladder muscle contracts to release urine when it receives signals from the brain that you’re at the toilet and ready to urinate. Those signals travel along the spinal cord and then get transmitted through the lower body to the bladder. Men and women with reflex incontinence suffer from detrusor overactivity, meaning that the muscle contracts at other times as well. When it does, urine can escape the bladder and leak out through the urethra. Usually, problems with the transmission of messages along the spinal cord are responsible for reflex urinary incontinence. As a result, healthcare providers sometimes refer to it as spinal or supraspinal reflex incontinence. Stroke is one of the main causes of reflex incontinence.
In addition to urinary incontinence, fecal incontinence can also occur. Fecal incontinence can manifest in uncontrolled bowel movements, difficulty getting to the toilet in time, or overflow due to constipation.
Understanding these various types is crucial for tailoring effective management strategies and enhancing the overall quality of life for stroke survivors dealing with incontinence.
How a Stroke Can Affect Bladder and Bowel Control
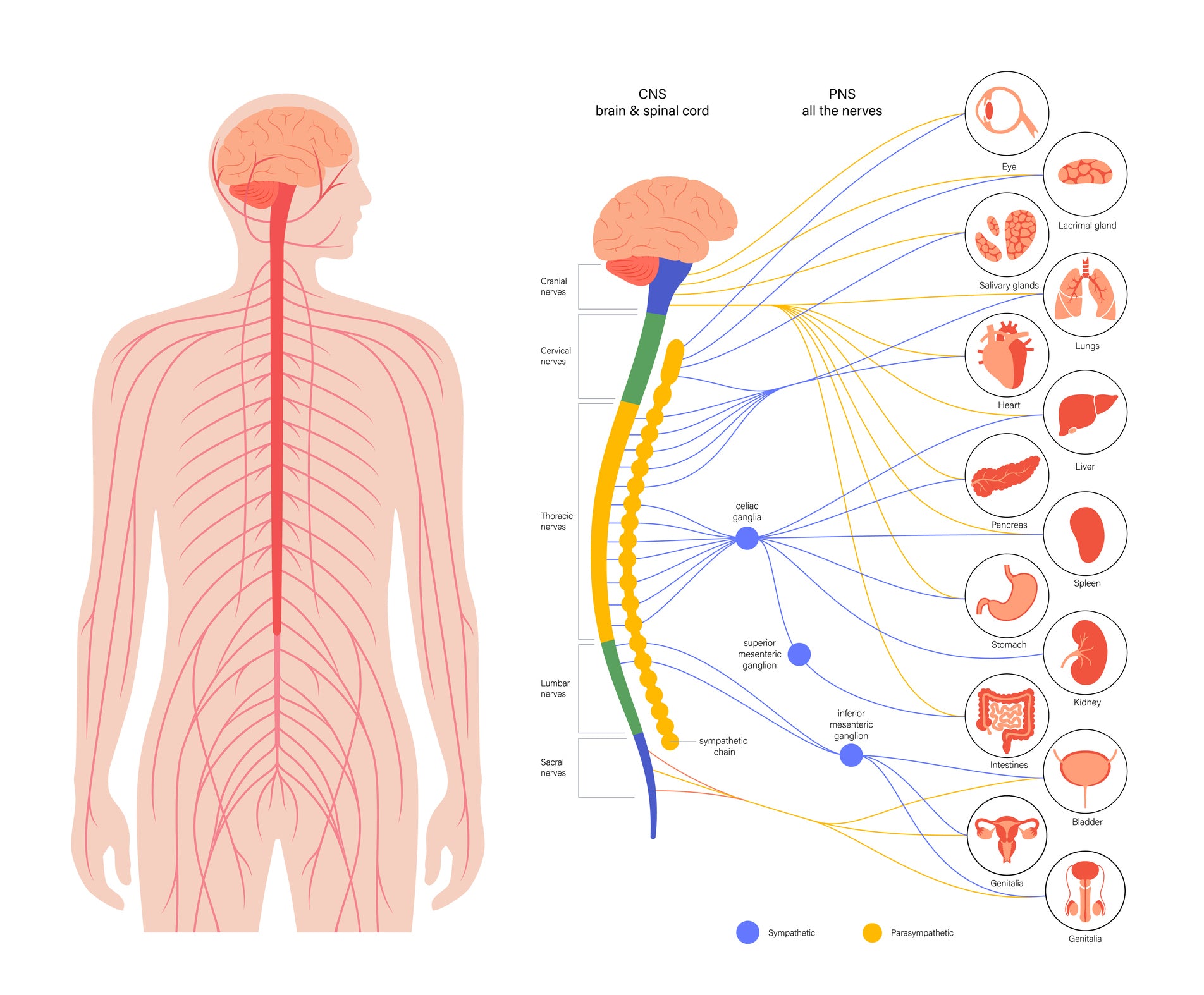
A stroke can significantly impact bladder and bowel control due to the neurological changes it induces. The brain plays a central role in regulating these functions, and when a stroke occurs, damage to specific areas may disrupt the communication between the brain and the muscles responsible for maintaining continence. This disruption can result in various challenges, such as weakened pelvic muscles, impaired nerve signals, or altered reflexes. The type and severity of the impact depend on the location and extent of the stroke.
In some cases, stroke survivors may struggle with maintaining voluntary control over urination or bowel movements, leading to forms of incontinence. Understanding the intricacies of how a stroke affects bladder and bowel control is crucial for developing targeted rehabilitation approaches and interventions to address these challenges in stroke recovery.
Common Signs and Symptoms of Stroke-Related Incontinence
Stroke-related incontinence manifests through various signs and symptoms that warrant attention for effective management. One common indicator is sudden, uncontrollable urges to urinate or defecate, often leading to accidental leakage. Individuals may also experience difficulty initiating or stopping the flow of urine or have inconsistent bowel movements. Leakage during activities such as coughing, sneezing, or lifting heavy objects is characteristic of stress incontinence.
Additionally, frequent urinary tract infections or persistent discomfort during urination may signal underlying incontinence issues. Cognitive challenges or physical impairments can contribute to functional incontinence, hindering the ability to reach the restroom in time. Recognizing these signs and symptoms is pivotal in promptly addressing stroke-related incontinence and tailoring effective interventions to enhance the overall quality of life for stroke survivors.

Practical Tips for Coping with Stroke Incontinence
Helpful Diet and Hydration Adjustments
Making thoughtful adjustments to diet and hydration can play a significant role in managing incontinence, including that which is associated with stroke. Maintaining a balanced and fiber-rich diet can contribute to regular bowel movements, reducing the risk of constipation, a common factor in incontinence. Adequate hydration is crucial to prevent concentrated urine and support overall bladder health. Monitoring and, if necessary, limiting the intake of caffeine and acidic foods can help mitigate irritation to the bladder, potentially alleviating urgency and leakage issues.
Additionally, individuals may find it beneficial to establish a consistent toileting schedule, promoting better bladder and bowel habits. Consulting with healthcare professionals, such as dietitians or urologists, can further guide personalized dietary adjustments tailored to the specific needs of those managing stroke-related incontinence.
Incorporating Bladder and Bowel Training Techniques
Incorporating bladder and bowel training techniques can be instrumental in effectively managing incontinence, especially in the context of stroke-related challenges. Bladder training involves scheduled and progressive voiding, helping individuals gradually extend the time between bathroom visits and regain better control over urination. Bowel training focuses on establishing a regular and predictable bowel movement routine, often synchronized with meals, to enhance consistency and reduce the likelihood of accidents.
Both techniques aim to retrain the muscles and nerves involved in bladder and bowel control. Kegel exercises, which target pelvic floor muscles, can also be beneficial in strengthening the muscles responsible for continence. Collaborating with healthcare professionals, such as physical therapists or continence advisors, can provide tailored guidance in implementing these techniques, offering a proactive approach to improving the management of incontinence following a stroke.
Utilizing Bladder Protection Products
Utilizing bladder protection products can be a practical and effective strategy for managing incontinence, particularly for individuals dealing with the aftermath of a stroke. These products, such as protective underwear (also known as adult diapers), pads and guards, or bed protectors, provide a discreet and reliable solution to contain and manage urinary or fecal leakage. They offer a sense of security, allowing individuals to engage in daily activities with confidence and without the fear of embarrassing accidents.
Choosing the right type of protection product depends on the specific needs and severity of incontinence. Incorporating these products into a comprehensive management plan can enhance the overall quality of life for individuals affected by stroke-related incontinence, providing both comfort and convenience in navigating daily routines. Health professionals can offer guidance on product selection and usage to optimize their effectiveness and ensure the best fit for individual circumstances
Making Environmental Adaptations for Enhanced Convenience and Comfort
Making environmental adaptations can significantly enhance convenience and comfort for individuals dealing with incontinence following a stroke. Simple adjustments in the living space, such as strategically placing accessible and easily reachable toileting facilities, can minimize the urgency and challenges associated with reaching the restroom in time. Installing handrails and grab bars in bathrooms can provide additional support, promoting safety during transfers and reducing the risk of accidents. Creating a well-lit and clutter-free environment can further contribute to improved mobility and visibility, aiding those with incontinence issues.
Additionally, having a contingency plan in place, such as keeping spare clothing and hygiene supplies readily available, can alleviate the stress of unexpected leaks. These thoughtful environmental adaptations not only enhance convenience but also foster a sense of independence and dignity for individuals managing incontinence post-stroke. Collaborating with occupational therapists or healthcare professionals can offer tailored guidance in optimizing the home environment to better suit the needs of those affected by stroke-related incontinence.
Building a Strong Support Network
Building a strong support network is a crucial aspect of coping with incontinence caused by a stroke. The challenges associated with managing incontinence can be both physical and emotional, making a reliable support system essential for individuals and their caregivers. Open communication with family, friends, and healthcare professionals fosters understanding and empathy, creating a safe space to discuss concerns and seek assistance. Caregivers play a vital role in providing practical support, from helping with daily tasks to offering emotional encouragement. Joining support groups or engaging in therapy sessions can connect individuals with others facing similar challenges, providing valuable insights, shared experiences, and a sense of community. Establishing a robust support network not only facilitates the practical aspects of managing incontinence but also contributes to emotional well-being, promoting resilience and an improved quality of life for those navigating the complexities of post-stroke incontinence.
If you're struggling with incontinence, join one of our private support groups today!
Women's Incontinence Support Group
Men's Incontinence Support Group

Caregiver Tips for Providing Compassionate Care
Providing compassionate care for someone with incontinence resulting from a stroke requires a thoughtful and understanding approach from caregivers. First and foremost, maintaining open communication is key, ensuring that both the caregiver and the individual feel comfortable discussing needs, concerns, and preferences related to incontinence management. Establishing a consistent routine for toileting and hygiene can help create predictability and minimize stress.
Offering emotional support and maintaining a non-judgmental attitude are crucial, as individuals may experience feelings of embarrassment or frustration. Being patient and allowing sufficient time for each step of the care process contributes to a more dignified and respectful caregiving experience. It's essential for caregivers to educate themselves on effective incontinence management techniques, including proper use of protective products and environmental adaptations.
Additionally, seeking respite and support for caregivers themselves is vital to prevent burnout and ensure sustainable, compassionate care for those affected by stroke-related incontinence.

Medical Interventions for Incontinence and Stroke
Medical interventions play a pivotal role in addressing incontinence associated with stroke. Healthcare professionals may employ a range of strategies to manage and improve urinary and bowel control in stroke survivors. Behavioral therapies, such as pelvic floor exercises and bladder training, are commonly recommended to enhance muscle strength and coordination. Medications, such as anticholinergics or alpha-blockers, may be prescribed to alleviate symptoms by affecting nerve signals or muscle contractions.
For more severe cases, minimally invasive procedures, such as bulkamid injections, or surgical interventions might be considered. Additionally, healthcare providers may explore neurostimulation techniques to modulate nerve activity and improve bladder function.
A comprehensive approach often involves collaboration between physicians, urologists, physical therapists, and other specialists to tailor interventions based on the specific needs and circumstances of the individual. Regular follow-up assessments allow for adjustments to the treatment plan, ensuring ongoing efficacy in managing incontinence following a stroke.
Sources:
Maree P. Williams, Velandai Srikanth, Margaret Bird, Amanda G. Thrift, Urinary symptoms and natural history of urinary continence after first-ever stroke—a longitudinal population-based study, Age and Ageing, Volume 41, Issue 3, May 2012, Pages 371–376, https://doi.org/10.1093/ageing/afs009
Harari D, Coshall C, Rudd AG, Wolfe CD. New-onset fecal incontinence after stroke: prevalence, natural history, risk factors, and impact. Stroke. 2003 Jan;34(1):144-50. doi: 10.1161/01.str.0000044169.54676.f5. PMID: 12511766.
Stroke Association. (2023, Jul.). Continence Problems. Stroke Association. https://www.stroke.org.uk/effects-of-stroke/physical-effects-of-stroke/continence-problems
American Stroke Association. (2019, Mar. 19). Incontinence. American Stroke Association. https://www.stroke.org/en/about-stroke/effects-of-stroke/physical-effects-of-stroke/physical-impact/incontinence
































