In recent years, vaginal mesh implants have been a topic of controversy, sparking debates on their safety and effectiveness in treating pelvic floor disorders. In this blog, we aim to provide a balanced perspective by exploring the differences between various types of vaginal mesh, shedding light on their unique characteristics, associated risks, and potential benefits. Join us as we navigate through the intricacies of vaginal mesh, empowering individuals with the knowledge they need to make informed decisions about their pelvic health.

Understanding Vaginal Mesh
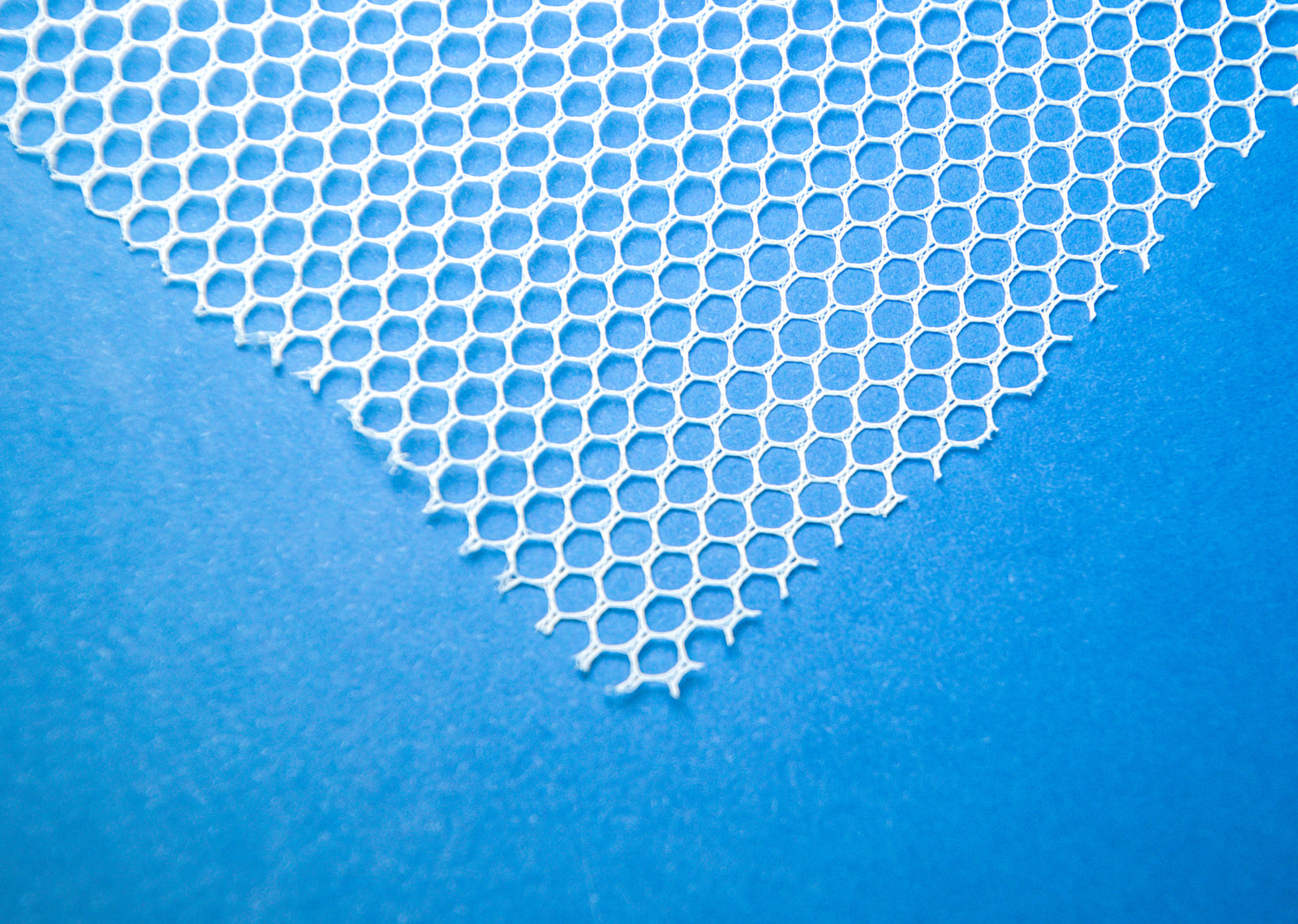
Vaginal mesh is a medical device used to reinforce weakened pelvic tissues and provide support for pelvic organs in conditions such as pelvic organ prolapse (POP) or stress urinary incontinence (SUI). There are three different types of mesh that have been used in this procedure either in the past or in current surgeries. These are:synthetic mesh, biologic mesh, and absorbable mesh.
Types of Vaginal Mesh Implants
- Synthetic Mesh: Made from materials such as polypropylene, synthetic mesh is durable and often used in surgical procedures for pelvic organ prolapse (POP)* or stress urinary incontinence (SUI).
- Biologic Mesh: Derived from animal or human tissue, biologic mesh is designed to integrate with the body's own tissues and is sometimes used as an alternative to synthetic mesh in pelvic floor surgeries.
- Absorbable Mesh: This type of mesh gradually dissolves and is absorbed by the body over time, providing temporary support during the healing process after pelvic floor surgery.
*Synthetic vaginal mesh products for transvaginal repair of pelvic organ prolapse (POP) are no longer available for sale in the United States. This decision was made by the U.S. Food and Drug Administration (FDA) in April 2019, citing concerns about the safety and effectiveness of these products.
Procedures Involving Vaginal Mesh
Vaginal mesh is primarily used in the surgical treatment of pelvic floor disorders, including pelvic organ prolapse (POP) and stress urinary incontinence (SUI). POP occurs when the muscles and tissues supporting pelvic organs weaken or stretch, causing organs such as the bladder, uterus, or rectum to protrude into the vaginal canal.
There are currently no FDA-approved surgical mesh products for transvaginal repair of prolapse marketed in the United States.
Sling procedures through the vagina, designed to provide additional support and reinforcement to the weakened pelvic tissues, restoring normal anatomy and alleviating symptoms such as pelvic pressure or bulging, are still considered the most effective treatment for stress incontinence. This procedure can be done with either synthetic mesh or human tissue. The FDA has not banned synthetic mesh for use in this procedure.
Laparoscopic repair provides the same support as a vaginally inserted sling procedure, but instead is inserted through small incisions on the abdomen. This positioning and process has been approved by the FDA and has not shown any significant complications.
Finally, patients may be eligible for a transvaginal prolapse repair with native tissue. This is a surgery to treat pelvic organ prolapse (POP) which uses the patient’s own tissue in place of synthetic mesh. This eliminates the complications from the banned synthetic mesh procedure.

Risks and Complications Associated with Vaginal Mesh
In this section, we'll examine the potential risks and complications associated with the use of vaginal mesh implants, shedding light on important considerations for individuals considering or undergoing pelvic floor surgery involving mesh.
Common Risks and Complications
Each type of mesh comes with different risks and complications and some are more risky than others.
Synthetic Mesh:
- Mesh Erosion: One of the most common complications, where the mesh erodes through the vaginal wall, leading to pain, discomfort, and infection.
- Infection: Risk of infection at the surgical site, which may require antibiotics or surgical intervention to treat.
- Pain: Persistent pelvic or vaginal pain, often due to mesh erosion, contraction, or nerve damage.
- Mesh Contraction: Mesh may shrink or contract over time, leading to discomfort, tightening, or distortion of surrounding tissues.
- Urinary Issues: Symptoms such as urinary frequency, urgency, or difficulty emptying the bladder may occur due to mesh compression or irritation of surrounding structures.
Biologic Mesh:
- Infection: Risk of infection at the surgical site, although less common compared to synthetic mesh.
- Allergic Reactions: Some individuals may experience allergic reactions to the animal or human tissue used in biologic mesh, leading to inflammation or discomfort.
- Recurrence of Prolapse: Biologic mesh may have a higher risk of prolapse recurrence compared to synthetic mesh due to its lower durability and strength.
- Mesh Absorption: In some cases, the body may absorb biologic mesh too quickly, leading to inadequate support and potential recurrence of prolapse.
Absorbable Mesh:
- Infection: Risk of infection at the surgical site, particularly during the absorption process when the mesh is breaking down.
- Foreign Body Reaction: The body's immune response to the absorbable mesh material may cause inflammation, discomfort, or swelling.
- Mesh Absorption Issues: Incomplete absorption or premature breakdown of the mesh may lead to inadequate support and potential recurrence of pelvic floor disorders.
- Delayed Complications: While absorbable mesh may initially seem to pose fewer risks, delayed complications such as erosion or contraction may still occur as the mesh degrades over time.
Complication Rates by Mesh Type & Procedure
- Mesh exposure: 1.7%
- Voiding dysfunction: 3.7%
- Overall complication rate: 8%
- Mesh Erosion: 10%
- Mesh exposure: 18%
- Overactive bladder: 52%
- Pelvic pain: 14%
- Overall complication rate: 15-25%
- Mesh erosion: 2%
- Overall complication rate: 2%
Potential Long-term Effects of Vaginal Mesh
The potential long-term effects of vaginal mesh implants remain a subject of ongoing research and debate within the medical community. While these implants can provide symptomatic relief for pelvic floor disorders in the short term, there are concerns regarding their safety and durability over time. Some individuals may experience complications such as erosion, chronic pain, urinary issues, or sexual dysfunction years after the initial surgery.
Additionally, there is limited data on the longevity of mesh implants and their effects on pelvic anatomy and function in the decades following placement. Long-term monitoring and further research are necessary to fully understand the implications of vaginal mesh use and to ensure the optimal management of pelvic floor disorders.
Benefits and Effectiveness of Vaginal Mesh
In this section, we'll delve into the benefits and effectiveness of vaginal mesh, particularly in the treatment of stress urinary incontinence (SUI).
Success Rates and Outcomes
In the treatment of stress incontinence, the success rate is around 70-90%.
In the treatment of prolapse with mesh, one study showed a success rate of 53%. However this study also found that 42% experienced mesh exposure, 39% experienced pain, and 20% experienced painful sex after.
When treating prolapse through sacrocolpopexy, the success rate is around 90%.

Alternatives to Vaginal Mesh
In this section, we'll explore alternative treatment options for pelvic floor disorders, providing individuals with comprehensive insights into non-mesh alternatives that offer relief from symptoms such as pelvic organ prolapse (POP) and stress urinary incontinence (SUI), while minimizing the risks associated with vaginal mesh implants.
Non-Surgical Alternatives for Pelvic Floor Disorders
Non-surgical alternatives for pelvic floor disorders offer viable options for individuals seeking relief from symptoms without the use of vaginal mesh implants. Pelvic floor physical therapy, combining exercises, manual therapy, and biofeedback techniques, has been shown to effectively strengthen pelvic muscles, improve bladder control, and alleviate symptoms of pelvic organ prolapse (POP) and stress urinary incontinence (SUI).
Additionally, lifestyle modifications such as weight management, dietary changes, and bladder training may also play a significant role in managing pelvic floor disorders and improving overall pelvic health.
Navigating the complexities surrounding vaginal mesh and pelvic floor disorders requires careful consideration of the risks, benefits, and available alternatives. While vaginal mesh implants may offer relief for some individuals with pelvic organ prolapse (POP) or stress urinary incontinence (SUI), they also carry potential risks and complications that warrant thorough discussion with healthcare providers.
Exploring non-surgical alternatives such as pelvic floor physical therapy and lifestyle modifications can provide effective symptom management while minimizing the risks associated with mesh implants.
Remember, if you suspect you may have pelvic organ prolapse or urinary incontinence, it's essential to speak to your doctor for proper evaluation, diagnosis, and personalized treatment recommendations tailored to your specific needs and circumstances.
Sources:
Carmel, M. (2022, Oct. 17). FDA ban on transvaginal mesh: What does it mean for women facing pelvic organ prolapse?, UT Southwestern Medical Center, https://utswmed.org/medblog/fda-ban-transvaginal-mesh-what-does-it-mean-women-facing-pelvic-organ-prolapse/
Bueno Garcia Reyes, P., & Hashim, H. (2020). Mesh complications: best practice in diagnosis and treatment. Therapeutic advances in urology, 12, 1756287220942993. https://doi.org/10.1177/1756287220942993
Barski, D., & Deng, D. Y. (2015). Management of Mesh Complications after SUI and POP Repair: Review and Analysis of the Current Literature. BioMed research international, 2015, 831285. https://doi.org/10.1155/2015/831285
(2020, Sept. 30). Surgical Mesh: Use and Complications in Women. The Cleveland Clinic, https://my.clevelandclinic.org/health/articles/16298-surgical-mesh-use-and-complications-in-women
Milani, A. L., Damoiseaux, A., IntHout, J., Kluivers, K. B., & Withagen, M. I. J. (2018). Long-term outcome of vaginal mesh or native tissue in recurrent prolapse: a randomized controlled trial. International urogynecology journal, 29(6), 847–858. https://doi.org/10.1007/s00192-017-3512-3
(2022, Oct. 12). Sacrocolpopexy. The Cleveland Clinic, https://my.clevelandclinic.org/health/treatments/17939-sacrocolpopexy