Can Obesity Cause Incontinence?
Obesity, standardly classified as having a body mass index BMI) of 30 or higher, is a risk factor for urinary incontinence. No matter what your age or gender, people who are obese are more likely to develop urinary incontinence. Estimates believe that 46% to 67% of obese women experience incontinence. Fortunately, there are methods to help. Learn how much obesity increases your chances of incontinence, why the connection exists, and how to eliminate or manage your incontinence.

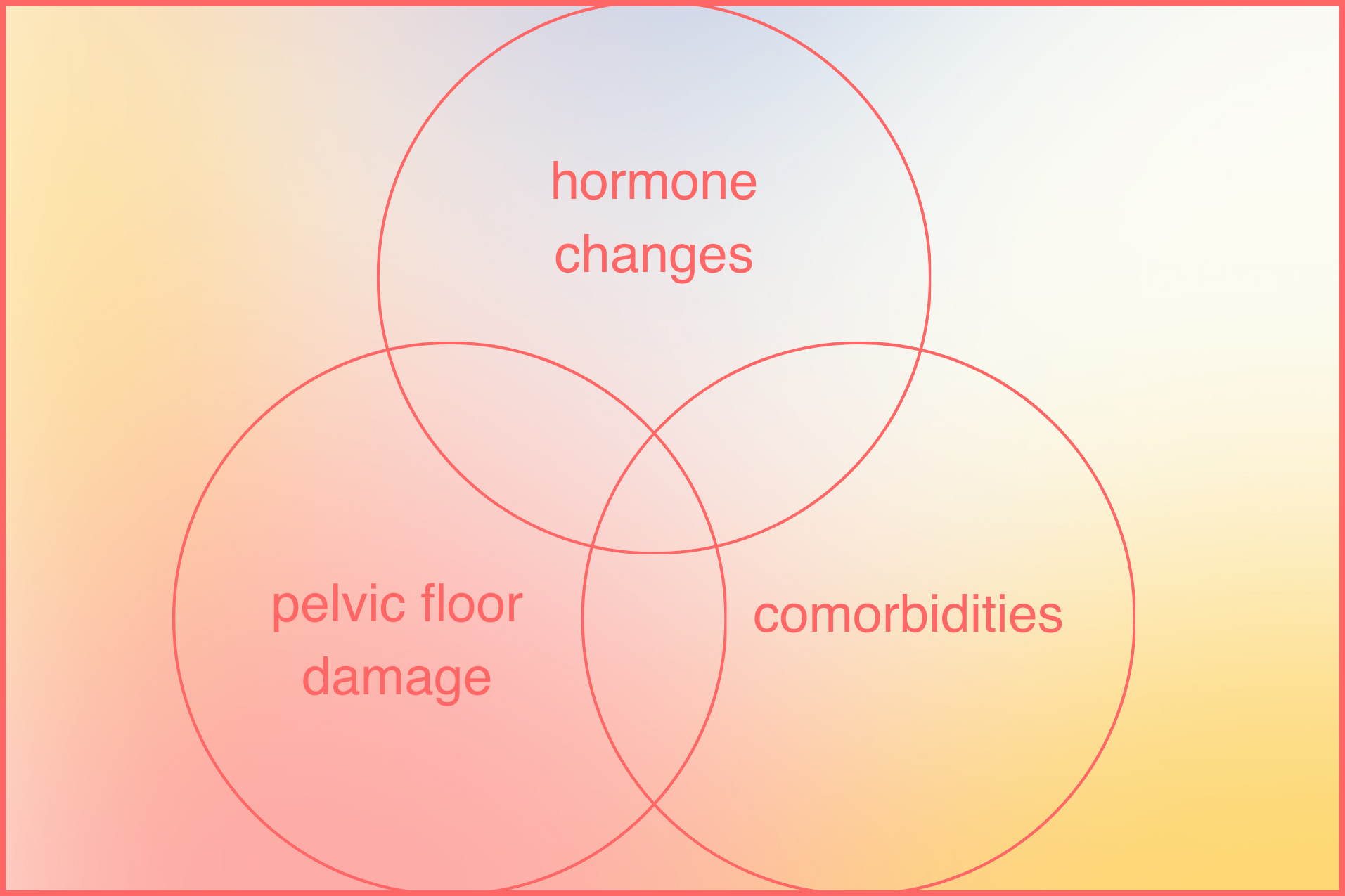
The Connection Between Obesity and Incontinence
There are several reasons obesity raises your risk for incontinence. Read more about the key connections between obesity and urinary incontinence below:
Pelvic Floor Pressure
Extra weight around the middle section puts pressure and stress on your pelvic floor. Your pelvic floor muscles and urethral structures can weaken and this can lead to accidental urine leaks. This weakening sometimes becomes more apparent when sneezing, coughing, or jumping.
Obesity-Related Hormonal Changes
As individuals gain excess weight, adipose tissue becomes a site for increased production of various hormones, including estrogen and leptin, while simultaneously altering the balance of other hormones like insulin. These hormonal shifts can lead to structural and functional changes in the pelvic floor muscles and connective tissues, weakening their ability to support the bladder and urethra.
Type 2 Diabetes
Obesity can also lead to Type 2 diabetes, which in turn causes a more frequent and urgent need to urinate. Type 2 diabetes damages the nerves that control your bladder, giving you less control over leaks. In addition, increased glucose levels in the blood can cause increased thirst and more frequent urination.
Medication Side Effects
Some medications, including those for diabetes, can cause fluid retention or a cough, both of which can worsen incontinence or increase the risk of bladder sensitivity. Increased thirst can be another common side effect from medications. While it’s crucial to stay hydrated, especially if you have incontinence, excess water increases your need to urinate.
The Impact of Obesity on Bladder Health
Obesity exerts a profound impact on bladder health across multiple dimensions. The excess accumulation of adipose tissue in obese individuals alters hormonal balance, leading to increased production of estrogen, leptin, and inflammatory cytokines, which can weaken the pelvic floor muscles and connective tissues. This weakening compromises the bladder's support structure, predisposing individuals to urinary incontinence and pelvic organ prolapse.
Moreover, obesity often accompanies comorbid conditions like diabetes mellitus, which can cause nerve damage and disrupt the intricate neural pathways regulating bladder function.
Additionally, the increased abdominal pressure resulting from excess weight places additional strain on the bladder, leading to urinary urgency, frequency, and incomplete emptying. Obesity-induced changes in metabolism and inflammation further exacerbate the risk of developing urinary tract infections and bladder stones.
Can Belly Fat Cause Frequent Urination?
Carrying excess body weight in your belly area or midsection can lead to more frequent urination and bladder leaks. Increased pressure on your abdominal area can worsen bladder pressure and affect the mobility of the urethra. This leads to worsening stress incontinence, and to a lesser extent, urge incontinence.

Will Losing Weight Help Urinary Incontinence?
Fortunately, if your incontinence is caused by obesity, this can be reduced significantly by following a healthy weight loss plan, diet, or surgery. In several observational studies of severely overweight women with incontinence, it’s been shown that, following bariatric surgery, the prevalence of stress urinary incontinence significantly decreased. Losing weight without surgery works the same way and provides long-term benefits in terms of urinary incontinence. For many people, weight gain is connected to other health issues, and therefore it may be challenging to lose weight. In this situation, the focus is on managing the symptoms of incontinence. Managing the symptoms of incontinence can help result in a more comfortable, hassle-free experience.
What Kind of Incontinence Does Obesity Cause?
Carrying excessive weight can lead to different types of urinary incontinence. According to a paper in Obesity Reviews, 70% of obese women showed signs of stress urinary incontinence. Stress incontinence, which occurs when you exert pressure on your bladder when coughing, sneezing, or exercising, can result from obesity due to excess weight in the midsection of your body. This can apply pressure on your pelvic floor, causing overactive bladder and increasing the likelihood of bladder leaks.

Tips for Managing Obesity Related Incontinence
Healthy Diet and Portion Control
A healthy diet and portion control play pivotal roles in managing obesity by promoting weight loss and overall well-being. Embracing a diet rich in whole foods, including fruits, vegetables, lean proteins, and whole grains, provides essential nutrients while reducing calorie intake. Incorporating fiber-rich foods helps promote satiety and regulates blood sugar levels, curbing cravings and overeating tendencies.
By adhering to appropriate portion sizes, individuals can foster healthier eating habits and foster mindful eating practices. Additionally, prioritizing nutrient-dense foods over calorie-dense options supports sustainable weight loss and long-term weight management.
Pelvic floor exercises
Pelvic floor exercises, commonly referred to as Kegels, can strengthen your pelvic floor and make incontinence more manageable. By contracting your pelvic floor muscles to close around your pelvic floor area and lift, you can bring awareness to those muscles to improve bladder control. Working on sustained holds and quick flicks with Kegels can help build these muscles and reduce incontinence over time. Pelvic floor exercises require no equipment and can be done whether you’re at home, in the office, or on-the-go.
Timed Voiding and Bladder training
Depending on your lifestyle and circumstances, bladder training could also be an effective method for managing obesity-related urge incontinence. During bladder training, you slowly increase the time between your bathroom breaks. For example, if you typically go to the bathroom every 30 minutes, you stretch it to 45 minutes, then an hour, etc. Over time, bladder training can lengthen the amount of time between bathroom trips, increase the capacity of your bladder, and diminish the sudden urge to urinate.
 Bladder Health Supplements
Bladder Health Supplements
Bladder health supplements can offer valuable support in managing and potentially alleviating symptoms of incontinence. These supplements often contain ingredients like cranberry extract, which may help prevent urinary tract infections by inhibiting bacterial adherence to the bladder wall.
Additionally, supplements containing pumpkin seed extract, saw palmetto, or soy extract may aid in strengthening pelvic floor muscles and improving bladder control. Some supplements also include probiotics, which help maintain a healthy balance of beneficial bacteria in the urinary tract, potentially reducing the risk of urinary tract infections and inflammation.
While bladder health supplements may not provide immediate or comprehensive relief from incontinence, when combined with lifestyle modifications and other treatment modalities, they can contribute to overall bladder health and symptom management.
Choosing the Right Bladder Protection Products
When it comes to preventing leaks, ensuring that you have well-fitting and comfortable incontinence underwear for day and night is key. To help make obesity-related incontinence more comfortable, look for the following when choosing incontinence underwear:
Incontinence underwear is designed to soak up urine to protect your skin and prevent leaks from showing through your clothing. However, not all incontinence underwear is designed with the same type of absorbent material. Look for underwear that is designed with an absorbent core to help absorb and contain leaks. Overnight underwear is frequently the most absorbent, and can be worn for up to 12 hours. Disposable bed protectors can also be helpful to prevent leaks from getting onto bedding or furniture.
Finding the right size of incontinence underwear for larger sizes can be difficult. Based on research, up to 50% of leaks can be caused by incorrect fit. To ensure underwear is both comfortable and leak-proof, consult the manufacturer’s size chart to ensure that the underwear fits comfortably around the waist. Few brands have sizing up to 2XL that will comfortably fit waist sizes up to 80 inches. Additionally, look for brands that reinforced leak guards around the leg holes to prevent leaks from escaping. Trying a few different brands for size and comfort may be the right solution before you commit to one product.
Take Care of Your Skin
Staying comfortable can be one of the biggest challenges of excessive body weight and incontinence. Excessive fat tissue, limited mobility, and skinfolds all contribute to skin issues in overweight adults, and proactive management of skin health should be a priority.
If you’re prone to sensitive skin, look for incontinence products that are designed to quickly absorb liquid and wick moisture away from the body. Keeping skin dry helps to protect it from irritation and possible infection.
Keeping moisture off the skin is the first step to preventing unwanted skin irritation. Warm, moist environments that can be found between skinfolds provide an ideal environment for microorganism growth. A common condition, candida albicans, also known as yeast, can grow out of control in these dark moist environments, leading to uncomfortable skin irritation. To prevent moisture from forming, avoid tight clothing, cleanse regularly with the help of disposable wipes, and inspect skin daily.
Intertrigo, or a rash in the body folds, can also be an uncomfortable symptom of obesity-related incontinence. To help maintain healthy skin in these areas, use a zinc-oxide based barrier cream to help protect the skin folds from irritation.
Finally, it is also common for adults with obesity to develop excess abdominal fat and skin leading to an abdominal pannus, or an abdominal fold. A large abdominal fold can lead to limited mobility, create unwanted pressure injury, and cause friction and chafing. Ensuring that the pannus stays dry, clean, and protected with the use of cleansing sprays, wipes, and barrier creams can help maintain proper skin health and comfort.
Medical Interventions and Treatments
Medical interventions and treatments for obesity-related incontinence encompass a range of approaches tailored to address the underlying causes and symptoms.
For individuals with severe obesity and incontinence resistant to lifestyle changes, surgical options like bariatric surgery may be considered to achieve significant weight loss and alleviate pressure on the bladder.
Additionally, medications such as anticholinergics or beta-3 adrenergic agonists may be prescribed to reduce bladder contractions and improve urine storage. In more complex cases, advanced interventions such as neuromodulation, where electrical stimulation is used to regulate bladder function, or injection therapies to support the urethra may be explored.
The choice of treatment depends on the severity of incontinence, individual health status, and patient preferences, underscoring the importance of personalized care and multidisciplinary approaches in managing obesity-related incontinence.
Manage your weight
In addition to choosing the right incontinence underwear, weight loss can be an effective long term solution to managing obesity related incontinence. Based on a recent study, study participants who lost 5-10% of their body weight had greater reductions in the frequency of urinary incontinence than those who did not experience weight loss. In addition to helping reduce the frequency of incontinence, modest weight losses of 5-10% are also helpful in reducing blood pressure and preventing diabetes. Working with your doctor to get a healthy weight loss plan in place can be a good first step to weight management for obesity-related incontinence.
When to Talk to Your Doctor
It's essential to engage in open dialogue with a healthcare professional about obesity-related incontinence as soon as symptoms arise or become bothersome. If you experience frequent or sudden urges to urinate, urine leakage during physical activity, or difficulty controlling your bladder, it's crucial to seek medical attention promptly.
Additionally, if obesity or weight gain coincides with the onset of urinary incontinence, discussing these changes with your doctor can help identify potential underlying causes and develop an appropriate treatment plan. Furthermore, if incontinence significantly impacts your quality of life, interferes with daily activities, or leads to embarrassment or discomfort, it's essential to address these concerns with a healthcare provider.
Early intervention and proactive management can help mitigate the impact of obesity-related incontinence, improve bladder health, and enhance overall well-being. Therefore, don't hesitate to initiate a conversation with your doctor to explore treatment options and strategies tailored to your individual needs and circumstances.
Do you or someone you’re caring for experience obesity-related incontinence? Take our Bladder Protection Quiz and get a starter pack for your loved one to try today!
If you're struggling with incontinence, join one of our private support groups today!
Women's Incontinence Support Group
Men's Incontinence Support Group
Sources:
Huang, A. J., Brown, J. S., Thom, D. H., Fink, H. A., Yaffe, K., & Study of Osteoporotic Fractures Research Group. (2009). Urinary incontinence in older community-dwelling women: the role of cognitive and physical function decline. Obstetrics and Gynecology, 113(2 Pt 1), 303-309. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2866035/Brown, J. S., Vittinghoff, E., Wyman, J. F., Stone, K. L., Nevitt, M. C., Ensrud, K. E., ... & Cummings, S. R. (2010). Urinary incontinence: does it increase risk for falls and fractures? Study of Osteoporotic Fractures Research Group. Journal of the American Geriatrics Society, 58(5), 721-729. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3038422/
































